Plan B might be needed for a number of reasons:
The principles behind good safety netting are simple.
All of these factors are key to the success of the safety netting process. Leaflets can be a very useful supplement to explanation and discussion. The opportunity to ask questions is also essential. Most importantly the parent should feel empowered to make an assessment and to return without feeling that they will be seen as over-anxious.
Recently, there was a lively discussion online (sparked by Damian Roland's writings about safety netting) about this subject, including some great tips about how to do it well and ways that it can go wrong. One of the pitfalls that were mentioned was the possibility that discussion about the appropriateness of the attendance might get in the way of the touchy-feely aspect of the safety netting. The gist was that if you discussed when not to come, this would be a barrier to appropriate attendance. While I agree that this can happen, I don't believe that by discouraging attendance we are running this risk, as long as it is all done in a positive way.
The idea that discussing appropriate attendance is inherently negative is based on a false assumption: namely that the parent wants to come to the doctor. Even where healthcare is free at the point of delivery there are many, many reasons why people do not want to see a doctor, with inconvenience being one of the most common.
Another issue is that the anxiety associated with the perceived need for a medical assessment is itself an unpleasant experience. I think that doctors under-appreciate this because we are made to feel like the hero of the hour. Someone was worried about a symptom and now we are the person to tell them that everything is almost certainly going to be fine. Go us!
Probably the most common example that I can think of is the way that parents often think that a cough and fever equals a chest infection. This is sometimes compounded by the belief that chest infection is often fatal - a rare outcome in a healthy child who is given appropriate treatment.
When I hear someone say that they have come to see me because they believe that their child has a chest infection and the child promptly runs off to play with the toys, I could be forgiven for having a 'why me?' moment. I could use this opportunity to explain why this is an inappropriate attendance since the child is so very well. That would be a tad self indulgent since I'm not the one with the worry. Instead, I should make sure that my consultation finishes on a positive note, with good safety netting advice that encourages re-attendance, right?
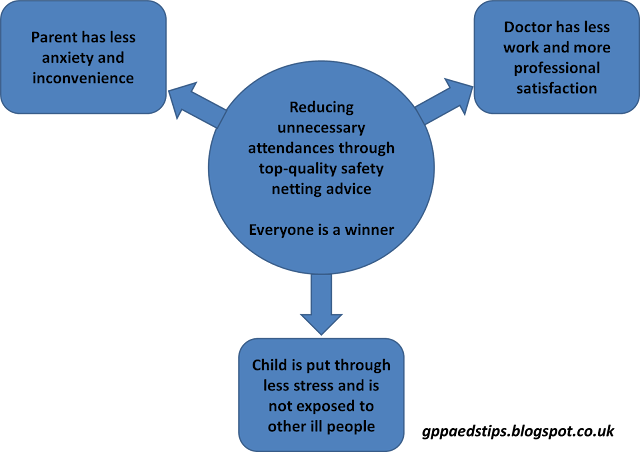
Well, I think that the two things (good safety netting and discouraging unnecessary attendances) are far from mutually exclusive.
If anything, the two things work together in beautiful harmony and create the opportunity to take safety netting to a platinum standard.
What might this look like in practice? For the child with the not-a-chest-infection, my school time safety netting might go like this:
It is absolutely important that parents do not feel criticised. If fear of criticism leads to a child not being brought for assessment when needed, that is of course a bad thing. So, we have to have the best of intentions when we talk about when and when not to seek medical advice.
I have no interest in doing myself out of a job by reducing attendances. If anything, reducing avoidable attendances. It takes me 2 minutes and zero stress to assess the child who has had a minor bump to the head. If the parents who bring their child to see me when all that's happened is that they fell over and cried for a few seconds stop coming "because it's always best to get checked isn't it doctor?" then I'll just have to see more patients that take time and challenge my thought processes. So why do I take the time to explain to every single parent the things that would constitute a reason to seek assessment for the next bumped head?
The answer is that it is in the best interests of the parent and child, so why wouldn't I?
Edward Snelson
Founder of MediLeaks
@sailordoctor
Disclaimer: Exploring health beliefs can be hazardous. Always wear a helmet.
I would love it if you would post the things that you educate parents about (in a positive way). You could do that here, on Twitter or on Facebook. If you post a comment here, don't worry if it doesn't appear straight away. I have to check all comments before they are published. (There are a lot of spammers out there!)