How can a paediatric subspecialty be so difficult and shrouded in mystery? Even the name, Child and Adolescent Mental Health Services, is complicated.
What do they do? The mystery extends to the online world of open-access medical education. Because I am putting together some resources for a university course at the moment, I went on my usual trawl for journal articles and online resources that might give me an idea about how we mere mortals should be doing our bit for child mental health problems. Compared to similar advice for asthma, sepsis or even just the limping child, there is virtually nothing out there for the clinician who recognises child mental health as a personal educational need.
What to do? Phone a friend. Yes, I spoke to an actual person. My expert told me that there are simple things that we can do to be a bit better at this. We need to ask more questions.
In order to do this we must enter the mind of a two and a half year old... ...or an ancient Greek philosopher. You decide.
If you've never taken a two and a half year old for a quick jolly down to the shops then you've really missed out. It goes something like this:
Socrates taught his students to question everything, including the answers to their questions. In this way, the answer behind what was superficially apparent comes to you. It's something that we all knew briefly when we were two and a half, but sometimes forget now that we are grown up and a bit dull. What is superficially apparent can seem to be the end point, but in child and adolescent mental health, it probably isn't.
Let me apply Socratic (if Socrates was two and a half) method to some common presentations to General Practice or the Emergency Department:
A 12 year old has abdominal pains that only occur during school terms.
Obvious answer: School avoidance.
Ask the question, "Why school avoidance?" - Answer: Anxiety symptoms due to undiagnosed dyslexia.
Obvious answer: School avoidance.
Ask the question, "Why school avoidance?" - Answer: Anxiety symptoms due to undiagnosed dyslexia.
A 13 year old is smoking cannabis every day.
Obvious answer: Bad parents and a chaotic home.
Ask the question, "Why?" - Answer: They have been having anxiety symptoms every day for nearly a year. Months ago, they were given some cannabis to try and they found that it helped take away that feeling. They started using it to feel more 'normal', not to get high.
Obvious answer: Bad parents and a chaotic home.
Ask the question, "Why?" - Answer: They have been having anxiety symptoms every day for nearly a year. Months ago, they were given some cannabis to try and they found that it helped take away that feeling. They started using it to feel more 'normal', not to get high.
A 15 year old has multiple symptoms for which there is no sensible medical explanation.
Obvious answer: Attention seeking
Ask the question, "Why?" - Answer: No obvious reason, so what else is going on?
Obvious answer: Attention seeking
Ask the question, "Why?" - Answer: No obvious reason, so what else is going on?
The list of things that young people present with that are viewed as behavioural include cutting/self-harming and anorexia. The reasons may be elusive, but they may also be identifiable. There may be a safeguarding issue.
Every one of these children deserve to have someone ask the question "why?"
In many cases they may not know why. They may not be able or ready to articulate it even if they do know. However, many young people can explain why they do what they do if someone is willing to give them a safe place to do so.
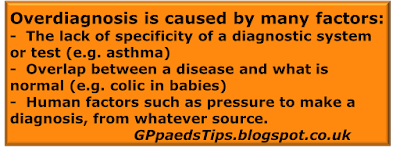
The important thing is to move away from making the obvious assumptions and instead always assume that there is more than meets the eye. The evidence is that mental health problems in young people are often not recognised.
In Emergency Medicine there is a saying, "The easiest injury to miss is the second one." That is equally true of child mental health. How do we make sure we always find the hidden problem? I don't know. Ask a two year old.