The quote "never tell me the odds" is from the late great Han Solo. His reckless approach to problem solving may not be the model that you strive for in clinical practice, but his attitude towards statistics is remarkably relevant in the context of diagnosing certain conditions in children.
Many of us have been taught to consider a personal or family history of atopy when making certain diagnoses in children. Although it might seem like this is an important factor, the logic for including the history of atopy has several flaws. It is notable that some guidelines are de-emphasising the value of such factors when considering a diagnosis of another atopic condition.
The first thing that is wrong with the use of the family history of atopy is that it is often itself wrong. We know that many diagnoses of asthma in children turn out to be wrong and that people can misinterpret what they were told. Were they given a diagnosis of asthma or were they told that their symptoms could possibly be due to asthma. Many patients don't understand what a maybe diagnosis is, no matter how comfortable we are with the concept. Similarly, there is much overdiagnosis of allergy, especially antibiotic allergy. The end result of all this is that there are many people with a history of an atopic condition but who never had that condition.
It is also worth factoring in that (depending on which study you read) there is a significant possibility that the stated father is not the biological father. It's not a major factor, but if we're going to consider odds, it is a factor.
The most important argument for me is to do with the way that the diagnosis is made. The question is, do you rely on something in the history in order to make a diagnosis? For example, a child presents with a fever and no clear focus. They have never left the UK in their life, so that pretty much rules out malaria.
Conversely, a ten year old child presents with a history of recurrent wheeze. This seems to have multiple triggers and is no just related to viral infections. The wheeze responds well to inhaled salbutamol. The child has never had eczema and neither parent has any history of any atopic conditions. Well that rules out asthma then doesn't it? Of course not.
The idea that a personal or family history of atopy should be a deciding factor may well be responsible for much of the overdiagnosis of certain conditions. For example, a three year old presents with four episodes of wheeze in the space of a few weeks. Each episode has been preceded by a runny nose and each has resolved over the course of a few days, with only a salbutamol inhaler for symptomatic treatment. The child's parent asks if the child has asthma. Both parents were given a diagnosis of asthma in childhood. Also, this child had eczema as a baby.
Already I can feel the gravitational pull of the asthma diagnosis. The personal and family history of atopy feel like compelling evidence, especially if we are slightly unsure about a diagnosis. However, it doesn't change the fact that the clinical picture is one of viral wheeze and not asthma. For this reason, the British Thoracic Society guidelines have de-emphasised the importance of the family history of atopy in diagnosing asthma in children. "The diagnosis of asthma in children and adults is based on the recognition of a characteristic pattern of
respiratory symptoms, signs and test results and the absence of any alternative explanation for these." (1)
When it comes to uncertain diagnoses, we are rarely more unsure of ourselves than when considering a diagnosis of non-IgE cow' milk protein allergy (CMPA). It doesn't help that there is no test that we can rely on or that the symptoms are all non-specific. CMPA, more than most diagnoses, relies very much on the recognition of a best-fit. Often and quite rightly, it is a diagnosis which is considered after other more likely diagnoses have been initially presumed. Should the infant having eczema or a parent with a history of atopy influence that process?
I think that there is no simple answer to this. What is certainly true is that just because a baby has eczema does not mean that their crying and regurgitation of feeds indicates a CMPA. Conversely, just because a child has no eczema and no family history of atopy does not mean that we should delay a cow's milk protein free trial if the clinical scenario suggests CMPA as a diagnosis.
What you really want to know now of course is the increase in statistical probability of CMPA which is associated with eczema and family history of atopy. I don't know the answer to that. If you know, keep it to yourself. Never tell me the odds.
Edward Snelson
Epidiminihilist
@sailordoctor
Disclaimer - Han Solo's death is in no way proof that you should know the odds. His long and successful career is proof enough that reckless and uninformed decision making is the best way to go about things.
Thursday, 26 October 2017
Wednesday, 11 October 2017
School Time Safety Netting
Safety netting is one of the most important interventions in acute paediatrics, whether you work in Primary or Secondary Care. When we give safety netting advice, it is usually in the context of a medical problem that we expect to run a benign course and then resolve. This is plan A. Safety netting advice allows us to inform the patient (or responsible carer) when to activate plan B.
Plan B might be needed for a number of reasons:
The principles behind good safety netting are simple.
All of these factors are key to the success of the safety netting process. Leaflets can be a very useful supplement to explanation and discussion. The opportunity to ask questions is also essential. Most importantly the parent should feel empowered to make an assessment and to return without feeling that they will be seen as over-anxious.
Recently, there was a lively discussion online (sparked by Damian Roland's writings about safety netting) about this subject, including some great tips about how to do it well and ways that it can go wrong. One of the pitfalls that were mentioned was the possibility that discussion about the appropriateness of the attendance might get in the way of the touchy-feely aspect of the safety netting. The gist was that if you discussed when not to come, this would be a barrier to appropriate attendance. While I agree that this can happen, I don't believe that by discouraging attendance we are running this risk, as long as it is all done in a positive way.
The idea that discussing appropriate attendance is inherently negative is based on a false assumption: namely that the parent wants to come to the doctor. Even where healthcare is free at the point of delivery there are many, many reasons why people do not want to see a doctor, with inconvenience being one of the most common.
Another issue is that the anxiety associated with the perceived need for a medical assessment is itself an unpleasant experience. I think that doctors under-appreciate this because we are made to feel like the hero of the hour. Someone was worried about a symptom and now we are the person to tell them that everything is almost certainly going to be fine. Go us!
Probably the most common example that I can think of is the way that parents often think that a cough and fever equals a chest infection. This is sometimes compounded by the belief that chest infection is often fatal - a rare outcome in a healthy child who is given appropriate treatment.
When I hear someone say that they have come to see me because they believe that their child has a chest infection and the child promptly runs off to play with the toys, I could be forgiven for having a 'why me?' moment. I could use this opportunity to explain why this is an inappropriate attendance since the child is so very well. That would be a tad self indulgent since I'm not the one with the worry. Instead, I should make sure that my consultation finishes on a positive note, with good safety netting advice that encourages re-attendance, right?
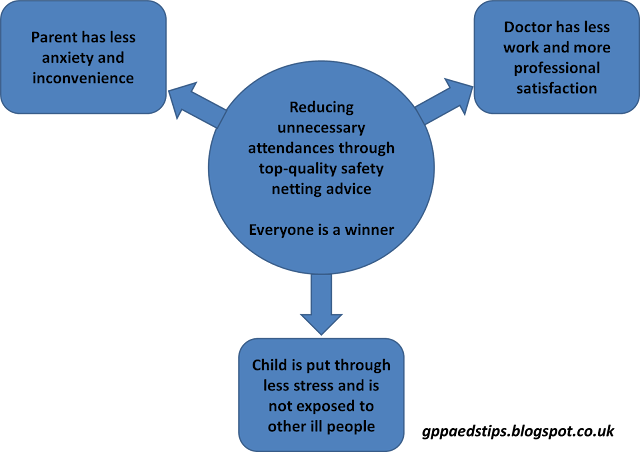
Well, I think that the two things (good safety netting and discouraging unnecessary attendances) are far from mutually exclusive.
If anything, the two things work together in beautiful harmony and create the opportunity to take safety netting to a platinum standard.
What might this look like in practice? For the child with the not-a-chest-infection, my school time safety netting might go like this:
It is absolutely important that parents do not feel criticised. If fear of criticism leads to a child not being brought for assessment when needed, that is of course a bad thing. So, we have to have the best of intentions when we talk about when and when not to seek medical advice.
I have no interest in doing myself out of a job by reducing attendances. If anything, reducing avoidable attendances. It takes me 2 minutes and zero stress to assess the child who has had a minor bump to the head. If the parents who bring their child to see me when all that's happened is that they fell over and cried for a few seconds stop coming "because it's always best to get checked isn't it doctor?" then I'll just have to see more patients that take time and challenge my thought processes. So why do I take the time to explain to every single parent the things that would constitute a reason to seek assessment for the next bumped head?
The answer is that it is in the best interests of the parent and child, so why wouldn't I?
Edward Snelson
Founder of MediLeaks
@sailordoctor
Disclaimer: Exploring health beliefs can be hazardous. Always wear a helmet.
I would love it if you would post the things that you educate parents about (in a positive way). You could do that here, on Twitter or on Facebook. If you post a comment here, don't worry if it doesn't appear straight away. I have to check all comments before they are published. (There are a lot of spammers out there!)
Plan B might be needed for a number of reasons:
The principles behind good safety netting are simple.
All of these factors are key to the success of the safety netting process. Leaflets can be a very useful supplement to explanation and discussion. The opportunity to ask questions is also essential. Most importantly the parent should feel empowered to make an assessment and to return without feeling that they will be seen as over-anxious.
Recently, there was a lively discussion online (sparked by Damian Roland's writings about safety netting) about this subject, including some great tips about how to do it well and ways that it can go wrong. One of the pitfalls that were mentioned was the possibility that discussion about the appropriateness of the attendance might get in the way of the touchy-feely aspect of the safety netting. The gist was that if you discussed when not to come, this would be a barrier to appropriate attendance. While I agree that this can happen, I don't believe that by discouraging attendance we are running this risk, as long as it is all done in a positive way.
The idea that discussing appropriate attendance is inherently negative is based on a false assumption: namely that the parent wants to come to the doctor. Even where healthcare is free at the point of delivery there are many, many reasons why people do not want to see a doctor, with inconvenience being one of the most common.
Another issue is that the anxiety associated with the perceived need for a medical assessment is itself an unpleasant experience. I think that doctors under-appreciate this because we are made to feel like the hero of the hour. Someone was worried about a symptom and now we are the person to tell them that everything is almost certainly going to be fine. Go us!
Probably the most common example that I can think of is the way that parents often think that a cough and fever equals a chest infection. This is sometimes compounded by the belief that chest infection is often fatal - a rare outcome in a healthy child who is given appropriate treatment.
When I hear someone say that they have come to see me because they believe that their child has a chest infection and the child promptly runs off to play with the toys, I could be forgiven for having a 'why me?' moment. I could use this opportunity to explain why this is an inappropriate attendance since the child is so very well. That would be a tad self indulgent since I'm not the one with the worry. Instead, I should make sure that my consultation finishes on a positive note, with good safety netting advice that encourages re-attendance, right?
Well, I think that the two things (good safety netting and discouraging unnecessary attendances) are far from mutually exclusive.
If anything, the two things work together in beautiful harmony and create the opportunity to take safety netting to a platinum standard.
What might this look like in practice? For the child with the not-a-chest-infection, my school time safety netting might go like this:
It is absolutely important that parents do not feel criticised. If fear of criticism leads to a child not being brought for assessment when needed, that is of course a bad thing. So, we have to have the best of intentions when we talk about when and when not to seek medical advice.
I have no interest in doing myself out of a job by reducing attendances. If anything, reducing avoidable attendances. It takes me 2 minutes and zero stress to assess the child who has had a minor bump to the head. If the parents who bring their child to see me when all that's happened is that they fell over and cried for a few seconds stop coming "because it's always best to get checked isn't it doctor?" then I'll just have to see more patients that take time and challenge my thought processes. So why do I take the time to explain to every single parent the things that would constitute a reason to seek assessment for the next bumped head?
The answer is that it is in the best interests of the parent and child, so why wouldn't I?
Edward Snelson
Founder of MediLeaks
@sailordoctor
Disclaimer: Exploring health beliefs can be hazardous. Always wear a helmet.
I would love it if you would post the things that you educate parents about (in a positive way). You could do that here, on Twitter or on Facebook. If you post a comment here, don't worry if it doesn't appear straight away. I have to check all comments before they are published. (There are a lot of spammers out there!)
Monday, 2 October 2017
It's Not Easy Being Wheezy - about antibiotics and wheezy kids
In my formative postgaduate years as a doctor, I was told by more than one mentor that antibiotics were a good treatment for children who were wheezing. This advice was given by various people at different times and whether this was bronchiolitis, viral wheeze* or an exacerbation of asthma, the principles seemed to be the same. The logic is sound - we know that infection triggers all three, and we can never be certain of the infection being a straightforward viral episode. That was how it was put to me anyway.
*If you are unsure about the difference between viral wheeze and bronchilitis, follow this link for an explanation.
I no longer believe in this strategy as a treatment option for wheezy kids, and this is why:
It's not easy being wheezy. Children with tight lower airways are up against it but often cope extremely well with their bronchospasm or their bronchiolitis. I am constantly delighted by the ability of these children to be cheerful despite quite significant breathing difficulty.
It's even worse to have a bacterial lower respiratory tract infection. As well as the breathing difficulty that comes from the loss of functioning lung, there is the tiring effect of the illness. Having pneumonia is unpleasant and often exhausting. It would be unusual to see a child who was cheerful and well despite a bacterial lower respiratory tract infection.
Now imagine combining the two. Doesn't look good does it? Children with bronchiolitis and viral wheeze cope with the difficulties of wet or constricted airways because they are systemically well. Add the lethargy of bacterial infection to this and you go from a child who can compensate to one who cannot. In short, you won't think "maybe there's a bacterial LRTI as well as the bronchiolitis or viral wheeze." You'll know it.
Evidence from research backs this up. The Cochrane review of antibiotics for bronchiolitis concluded that there was no benefit from antibiotics. (1)
You could say, what's the harm in trying antibiotics? There are many reasons why unnecessary antibiotics might be harmful and none of these are to do with drug resistance.
So, it's time to do away with the idea that antibiotics have a role in treating well children with bronchiolitis or viral wheeze. I believe that you'll know the children who need antibiotics because they will be properly unwell.
Edward Snelson
Antibiotic Guardian of the Galaxy
@sailordoctor
Reference
*If you are unsure about the difference between viral wheeze and bronchilitis, follow this link for an explanation.
I no longer believe in this strategy as a treatment option for wheezy kids, and this is why:
It's not easy being wheezy. Children with tight lower airways are up against it but often cope extremely well with their bronchospasm or their bronchiolitis. I am constantly delighted by the ability of these children to be cheerful despite quite significant breathing difficulty.
It's even worse to have a bacterial lower respiratory tract infection. As well as the breathing difficulty that comes from the loss of functioning lung, there is the tiring effect of the illness. Having pneumonia is unpleasant and often exhausting. It would be unusual to see a child who was cheerful and well despite a bacterial lower respiratory tract infection.
Now imagine combining the two. Doesn't look good does it? Children with bronchiolitis and viral wheeze cope with the difficulties of wet or constricted airways because they are systemically well. Add the lethargy of bacterial infection to this and you go from a child who can compensate to one who cannot. In short, you won't think "maybe there's a bacterial LRTI as well as the bronchiolitis or viral wheeze." You'll know it.
Evidence from research backs this up. The Cochrane review of antibiotics for bronchiolitis concluded that there was no benefit from antibiotics. (1)
You could say, what's the harm in trying antibiotics? There are many reasons why unnecessary antibiotics might be harmful and none of these are to do with drug resistance.
So, it's time to do away with the idea that antibiotics have a role in treating well children with bronchiolitis or viral wheeze. I believe that you'll know the children who need antibiotics because they will be properly unwell.
Edward Snelson
Antibiotic Guardian of the Galaxy
Reference
Subscribe to:
Comments (Atom)